
Overview
There are two options for obtaining a Blue Cross provider record:
As a participating facility and hospital, you:
As a Non-participating Provider, you:
Credentialing Process
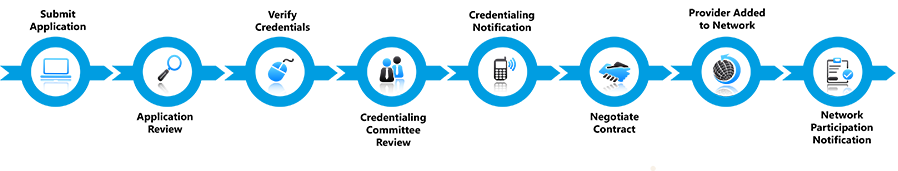
The credentialing process can take up to 90 days after all required information is received. Providers will remain non-participating in our networks until their application has been approved by the credentialing committee. The committee approves credentialing twice per month. After 90 days, you may inquire about your credentialing status by contacting our Provider Credentialing & Data Management Department at pcdmstatus@bcbsla.com.
The following facility provider types must meet certain criteria requirements to participate in our networks:
Learn more about Facility Provider type requirements.
Join Our Network
Your request can take up to 90 days to process once all required information has been received. The BCBSLA Welcome to the Network notification letter will notify you of next steps and your network participation effective date shall be the effective date indicated on the signature page of your provider agreement. Louisiana Blue does not backdate network participation. Any claims submitted prior to network participation will process as out-of-network. When a claim is processed as out-of-network, payment for services may go to the member not to the provider.
Applying for network participation has been made easy. Our online Facility Initial Credentialing packet can now be completed, signed and submitted digitally with DocuSign. Each packet includes a checklist of all required documents. Please follow that checklist to ensure all information is included with the submission of your application.
Facility Initial Credentialing Packet
Some of the required credentialing supporting documentation for Facilities and Hospitals includes:
Network facilities and hospitals are reverified every three years from their last credentialing acceptance date. Blue Cross sends reverification packets directly to facilities and hospitals based on the correspondence information on file.
Need Help with DocuSign®?
Many of our applications and forms must be completed, signed and submitted digitally through DocuSign® only. This electronic method reduces the need to print and submit hardcopy documents. For details on completing DocuSign forms, view this guide.
Update Your Information
Please note, providers are considered out of network until they receive the BCBSLA Welcome to the Network notification letter. The BCBSLA Welcome to the Network notification letter will notify you of next steps and your network participation effective date shall be the effective date indicated on the signature page of your provider agreement. Louisiana Blue does not backdate network participation. Any claims submitted prior to network participation will process as out-of-network. When a claim is processed as out-of-network, payment for services may go to the member not to the provider.
Maintaining information within your provider record is a key piece to participating in Blue Cross and Blue Shield of Louisiana provider networks or obtaining a provider record. It is important that you keep us abreast of any changes to the information in your record. This allows us to keep our directories current, contact you when needed as well as disperse payments. These forms are in DocuSign® format, allowing you to easily submit them to Louisiana Blue electronically.
Provider Update Request Forms – to update information such as:
Need Help with DocuSign®?
Many of our applications and forms must be completed, signed and submitted digitally through DocuSign® only. This electronic method reduces the need to print and submit hardcopy documents. For details on completing DocuSign forms, view this guide.
Frequently Asked Questions
The following forms can be found on our Provider page at www.bcbsla.com/providers, click on “Resources,” and look under the “Forms” section.